Title
題目
An End-to-End Geometry-Based Pipeline forAutomatic Preoperative Surgical Planning ofPelvic Fracture Reduction and Fixation
用于骨盆骨折復位與固定自動術前手術規劃的基于幾何的端到端流水線
01
文獻速遞介紹
骨盆骨折及其術前規劃相關研究背景與本文方法 骨盆骨折是一種常見的嚴重創傷,主要由高能量外力導致[1],約占所有骨折類型的1%–3%。超過50%的骨盆骨折患者會出現并發癥及多發損傷,包括閉合性顱腦損傷、盆腔血管出血和敗血癥等。其中,開放性骨盆骨折的致死率預計高達30%–50%[2]。多數情況下,骨折碎片移位越嚴重,盆腔出血的可能性越高,而盆腔出血正是骨盆骨折患者的首要死亡原因[3]。 骨折復位手術作為最常見的手術方式之一[4],是恢復骨盆骨折患者受損運動功能的有效治療手段[5]。該手術通常分兩步進行:1)將移位的骨折塊復位至解剖學位置;2)采用螺釘、鋼板等內固定器械對骨折部位進行固定,以維持復位后的穩定狀態。若骨盆結構的解剖關系未完全恢復,或固定效果不可靠,可能引發創傷性骶髂關節/髖關節骨關節炎、骨折再次移位等遠期疾病[6];患者還可能出現腰痛、步態異常或其他功能障礙等后遺癥,嚴重影響工作與日常生活[7]。因此,骨折復位與內固定的術前規劃至關重要。 然而,傳統基于外科醫生臨床經驗與操作習慣的規劃方式存在諸多問題,如術中需反復調整方案、手術時間延長、術中透視輻射暴露過量等[8]。計算機輔助術前規劃可有效規避上述問題,但在骨盆骨折場景中,骨折類型的多樣性以及細小骨折碎片可能造成的干擾,導致骨骼分割與配準難度顯著增加,為規劃帶來新挑戰。現有計算機輔助系統多僅針對規劃流程中的部分環節,且往往需要人工干預以確保規劃精度。據作者所知,目前尚未有完整的端到端自動化術前規劃方法被提出。 ?本文提出一種針對骨盆骨折全流程術前規劃的全自動端到端計算機輔助方法,主要貢獻包括三點:1)首個融合分割、復位與植入規劃的骨盆骨折全自動端到端術前規劃方法;2)提出一種新的兩步式形態學自動配準方法,該方法結合對稱特征與面特征,符合臨床復位手術標準;3)提出一種迭代幾何方法以計算近最優植入位置,并改進了帶多約束的密集搜索優化算法以確定植入方向。 本方法是首個融合分割、復位與植入規劃的骨盆骨折端到端術前規劃方案,可大幅簡化傳統術前規劃中繁瑣的流程,為外科醫生提供便利。
Abatract
摘要
Computer-assisted preoperative planning ofpelvic fracture reduction surgery has the potential toincrease the accuracy of the surgery and to reduce complications. However, the diversity of the pelvic fracturesand the disturbance of small fracture fragments present agreat challenge to perform reliable automatic preoperativeplanning. In this paper, we present a comprehensive andautomatic preoperative planning pipeline for pelvic fracturesurgery. It includes pelvic fracture labeling, reduction planning of the fracture, and customized screw implantation.First, automatic bone fracture labeling is performed basedon the separation of the fracture sections. Then, fracturereduction planning is performed based on automatic extraction and pairing of the fracture surfaces. Finally, screwimplantation is planned using the adjoint fracture surfaces.The proposed pipeline was tested on different types ofpelvic fracture in 14 clinical cases. Our method achieveda translational and rotational accuracy of 2.56 mm and3.31? in reduction planning. For fixation planning, a clinical acceptance rate of 86.7% was achieved. The resultsdemonstrate the feasibility of the clinical application of ourmethod. Our method has shown accuracy and reliabilityfor complex multi-body bone fractures, which may provideeffective clinical preoperative guidance and may improvethe accuracy of pelvic fracture reduction surgery.
計算機輔助骨盆骨折復位手術術前規劃的研究 計算機輔助骨盆骨折復位手術術前規劃,有望提高手術精準度并減少并發癥。然而,骨盆骨折類型的多樣性以及細小骨折碎片的干擾,為實現可靠的自動化術前規劃帶來了巨大挑戰。 本文提出了一套全面的骨盆骨折手術自動化術前規劃流程,涵蓋骨盆骨折標記、骨折復位規劃及個性化螺釘植入規劃三個核心環節:首先,基于骨折斷端的分離情況實現骨折自動標記;其次,通過骨折面的自動提取與配對完成骨折復位規劃;最后,利用相鄰骨折面進行螺釘植入規劃。 該規劃流程在14例臨床病例的不同類型骨盆骨折中進行了測試。結果顯示,在復位規劃方面,平移精度與旋轉精度分別達到2.56毫米和3.31度;在固定規劃方面,臨床接受率達86.7%。這些結果證實了該方法臨床應用的可行性。此外,該方法對復雜多體骨骨折展現出良好的精準度與可靠性,有望為臨床提供有效的術前指導,并提升骨盆骨折復位手術的精準度。
Method
方法
A. Overview
Fig. 1 shows the pipeline of our preoperative planningmethod. The input is the CT scan of the patient’s pelvicstructure. The outputs are the bone fragments, their spatiallocation, the implants, and their spatial location. And itconsists of 3 stages: Stage I is an automatic method forlabeling fracture fragments, which identifies and separatesall the bone fragments based on the improved adaptive-levelwatershed algorithm [35]. Subsequently, triangular meshes andpoint clouds of the fragments are generated as the input forthe subsequent stages; Stage II computes the target pose ofbone fragments by a proposed two-step surgical reductionmethod. The first step is the registration to the mirroredcontralateral bone based on the fast point feature histogram(FPFH) registration algorithm [36]. The second step is theautomatic registration based on fracture surfaces; Stage IIIis a novel personalized planning method of fracture fixationby screw implantation with several proposed geometry-basedalgorithms, based on the fracture surface computed in StageII. The planning of implantation includes the computation ofthe screws’ implanting amount, position, and direction.
A. 概述 圖1展示了我們術前規劃方法的流程。輸入數據為患者骨盆結構的計算機斷層掃描(CT)圖像,輸出結果包括骨折塊及其空間位置、植入物及其空間位置。該流程包含3個階段: ? 1. 階段I(骨折塊標記):一種自動化的骨折塊標記方法,基于改進的自適應水平分水嶺算法[35]識別并分離所有骨折塊。隨后,生成骨折塊的三角網格和點云,作為后續階段的輸入數據; ? 2. 階段II(骨折復位規劃):通過提出的兩步手術復位方法計算骨折塊的目標位姿。第一步是基于快速點特征直方圖(FPFH)配準算法[36],將骨折塊與鏡像對側骨骼進行配準;第二步是基于骨折面的自動配準; ? 3. 階段III(螺釘植入規劃):一種新穎的個性化骨折固定規劃方法,基于階段II計算得到的骨折面,采用多種提出的幾何算法規劃螺釘植入方案。植入規劃包括計算螺釘的植入數量、位置和方向。
Conclusion
結論
In this work, we proposed an automatic preoperative planning method for pelvic fracture reduction surgery that consistsof three stages. The fracture fragment labeling method is basedon the separation of fracture sections. For the reduction planning, a two-step registration is used to compute the anatomicalposition of the fractured bones. Finally, an implantation planof the number, positions, and directions of implanted screwsis generated based on the adjoint fracture faces. All threestages of preoperative planning of pelvic fracture surgery canbe automatically performed with little or no user interaction.Experiments on clinical datasets from a publicly availabledataset demonstrate the feasibility of our method. More clinical data will be collected to verify the stability and improvethe detailed design of the pipeline, and to extend our methodto other types of fractures in the future.
本文研究內容摘要 本研究提出一種適用于骨盆骨折復位手術的自動術前規劃方法,該方法包含三個階段: ? 1. 骨折塊標記階段:基于骨折斷面分離實現骨折塊標記; ? 2. 復位規劃階段:采用兩步配準法計算骨折塊的解剖學位置; ? 3. 植入規劃階段:依據相鄰骨折面生成螺釘植入數量、位置及方向的規劃方案。 ? 骨盆骨折手術術前規劃的上述三個階段均可自動完成,幾乎無需或完全無需用戶干預。 ? 基于公開數據集的臨床數據實驗驗證了該方法的可行性。未來,研究團隊將收集更多臨床數據,以驗證該方法的穩定性、改進流程的細節設計,并將其擴展應用于其他類型的骨折(手術術前規劃)。
Figure
圖
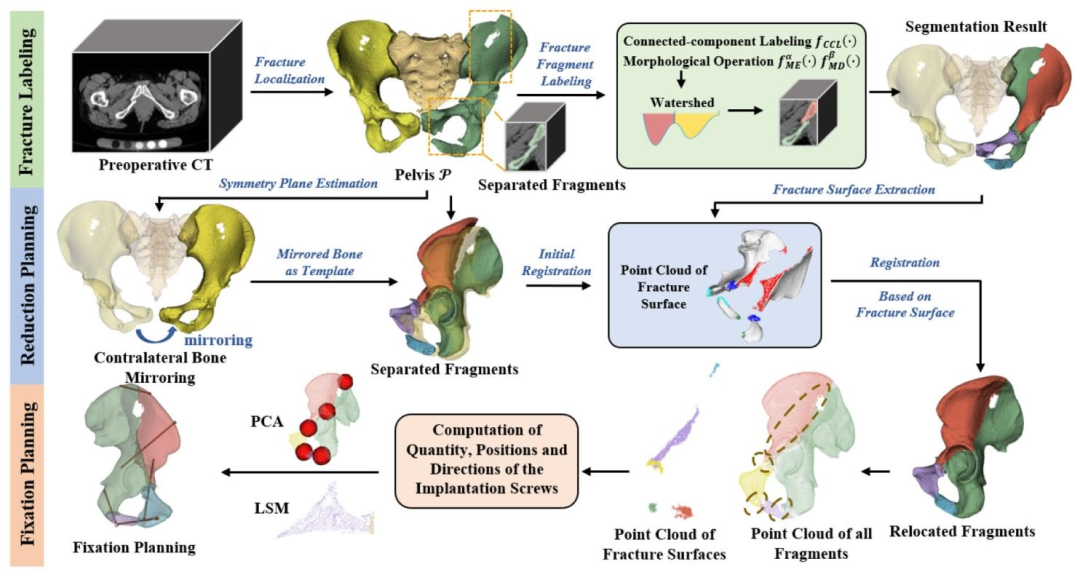
Fig. 1. Pipeline of the preoperative planning method for pelvic fracture surgery. StageI: Bone Fracture Labeling; StageII: Fracture ReductionPlanning; StageIII: Fixation Planning
圖1 骨盆骨折手術術前規劃方法流程 該流程分為三個階段: ? - 第一階段(Stage I):骨折標記(Bone Fracture Labeling) ? - 第二階段(Stage II):骨折復位規劃(Fracture Reduction Planning) ? - 第三階段(Stage III):固定規劃(Fixation Planning)
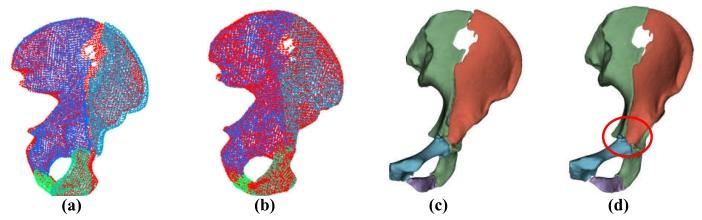
Fig. 2. Illustration of the effect of coarse registration: (a)-(b) relativeposition of P T (red) and ?P1, · · · ,Pn ?before and after registration;(c)-(d) F1, · · · , Fn ?before and after registration.
圖2 粗配準效果示意圖 - (a)-(b):配準前后,目標骨盆((P_T),紅色標記)與待配準骨盆((P_1,···,P_n))的相對位置關系; - (c)-(d):配準前后,待配準骨盆對應的骨折面((F_1,···,F_n))的狀態變化。
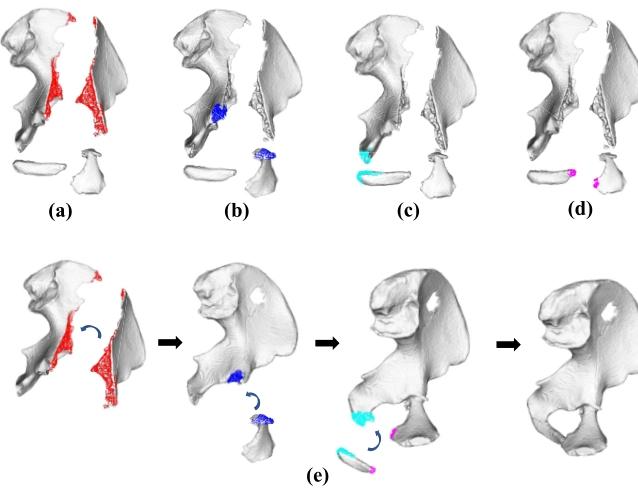
Fig. 3. Registration based on pairwise point clouds. (a)-(d) Pairwise pointclouds of fracture surfaces. Each color of the point cloud corresponds toa matching pair of point clouds; (e) The progress of the registration basedon the point clouds of the fracture surface.
圖3 基于點云配對的配準過程 - (a)-(d):骨折面的點云配對結果,點云中的每種顏色對應一組匹配的點云對; - (e):基于骨折面點云的配準進度(或動態過程)展示。
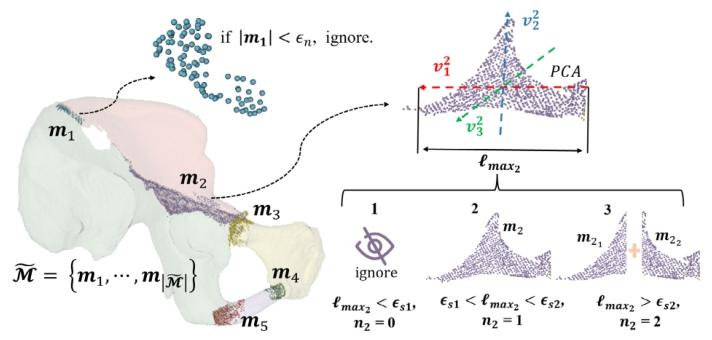
Fig. 4. Illustration of the computation of the number of implanted screwsfor fragments m1 and m2.
圖4 骨折塊m?與m?的植入螺釘數量計算示意圖 ?
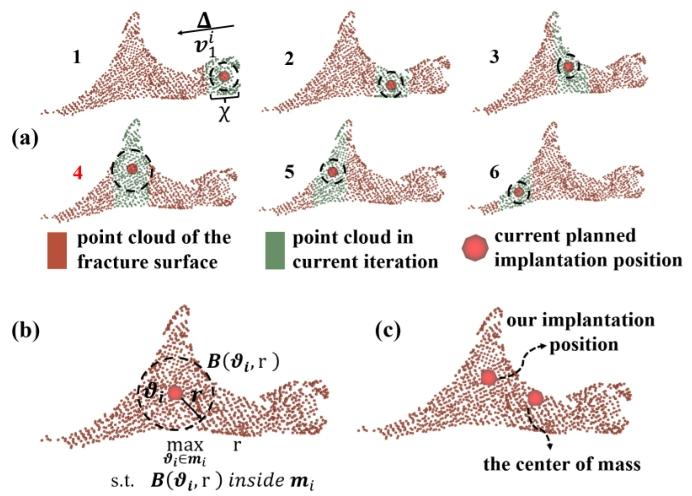
Fig. 5. Illustration of the computation of the positions of the implantedscrews. (a) iterative computation process; (b) the ideal implantationposition; (c) a comparison of our planned position and the center of mass.
圖5 植入螺釘位置計算示意圖 - (a):螺釘位置的迭代計算過程(展示通過多輪迭代優化,逐步逼近最優螺釘位置的動態步驟); - (b):螺釘的理想植入位置(呈現符合臨床固定需求、兼顧穩定性與安全性的目標位置); - (c):本文規劃的螺釘位置與質心位置的對比(通過直觀對比,驗證所提方法規劃位置相較于質心位置的合理性與優勢)。
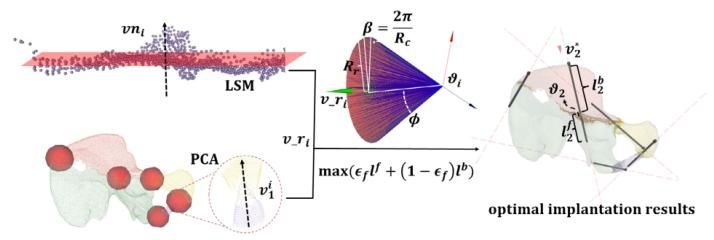
Fig. 6. Illustration of the computation of the directions of the implantedscrews. For an implantation position, an initial direction vri is generatedaccording to the point cloud in and around the fracture surface. Thenwith vri , an improved dense search method based on [40] is proposed toobtain the optimal trajectory
圖6 植入螺釘方向計算示意圖 對于某一植入位置,首先根據骨折面內部及周邊的點云生成初始方向(v_r_i);隨后以(v_r_i)為基礎,采用一種基于文獻[40]改進的密集搜索方法,最終確定螺釘的最優植入軌跡。
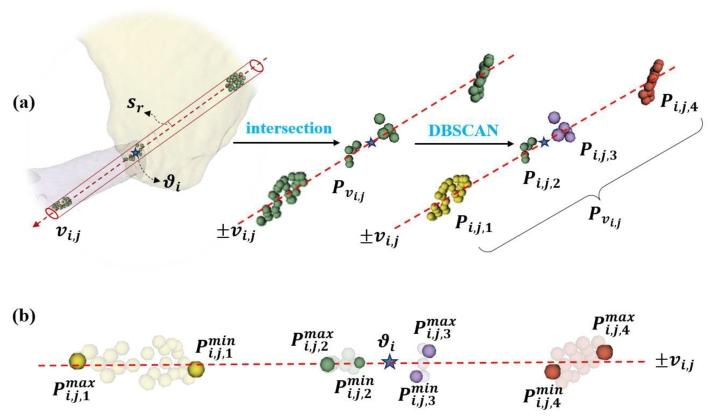
Fig. 7. Illustration of: (a) the extract and the clustering of the points insidethe cylinder passing through ?i with vi,j as the axis, sr as the radius; (b)computation of the closest and farthest points from ?i in each category,where πmini,j,1 = p min i,j,1 ? ?i , πi max ,j,1 = p max i,j,1 ? ?i
圖7 相關計算過程示意圖 - (a):以(v{i,j})為軸線、(s_r)為半徑,對穿過點(\vartheta_i)的圓柱體內的點進行提取與聚類(展示從特定幾何范圍內篩選目標點,并通過聚類算法分組的過程); - (b):計算每類點中與(\vartheta_i)距離最近和最遠的點,其中(\pi{i,j,1}^{\text{min}} = p{i,j,1}^{\text{min}} - \vartheta_i),(\pi{i,j,1}^{\text{max}} = p_{i,j,1}^{\text{max}} - \vartheta_i)(呈現對聚類后各組點的距離量化計算,明確近點與遠點相對于(\vartheta_i)的偏移關系)。
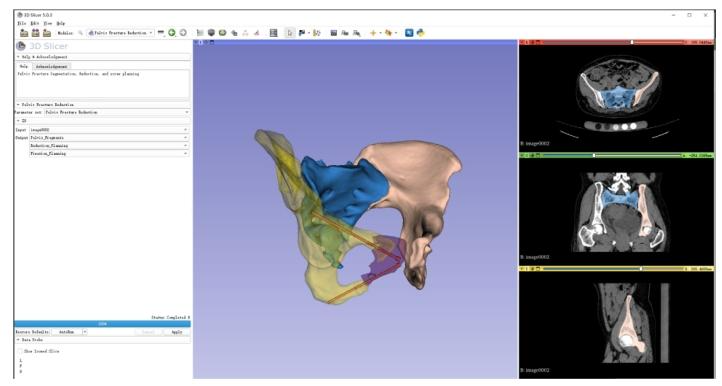
Fig. 8. Our preoperative planning system on 3D Slicer is implemented inan extensible module that allows for advanced functionality in fragmentlabeling, reduction planning, and screw implantation planning. The inputis a preoperative CT image. It allows visualization of the post-reductionpositions of the individually labeled fragments and the position andlocation of the screws (in red)
圖8 基于3D Slicer的術前規劃系統 該術前規劃系統在3D Slicer平臺上以可擴展模塊形式實現,具備骨折塊標記、復位規劃及螺釘植入規劃的高級功能。系統輸入為術前CT圖像,可可視化展示:經單獨標記的各骨折塊復位后的位置,以及螺釘(紅色標記)的植入位置與方位。
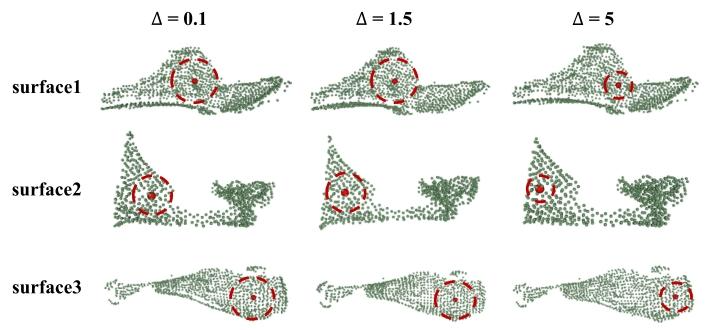
Fig. 9. Illustration of the results of the sensitivity study on the step size ?for computing Chebyshev Center with Equations 14-18. The maps showthe three fracture surfaces from different pelvis in different locations,scales, and shapes
圖9 基于式(14-18)計算切比雪夫中心時步長?的敏感性研究結果示意圖 圖中展示了來自不同骨盆、處于不同位置、具有不同尺度與形態的三個骨折面,用于呈現步長?的變化對切比雪夫中心計算結果的影響(以此驗證步長參數選擇對算法穩定性或精度的敏感程度)。
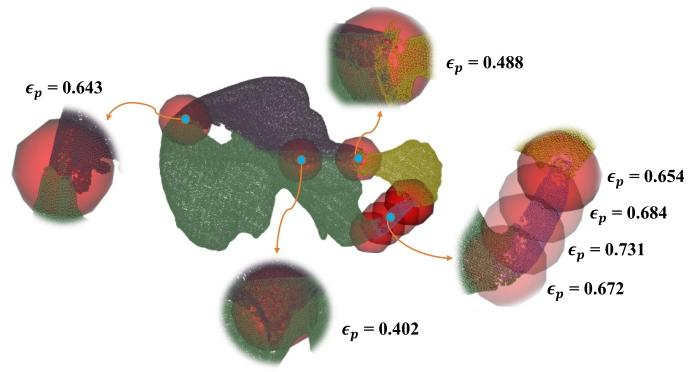
Fig. 10. The results of the exploratory study on principal componentcontribution values in different regions of the pelvis
圖10 骨盆不同區域主成分貢獻值的探索性研究結果
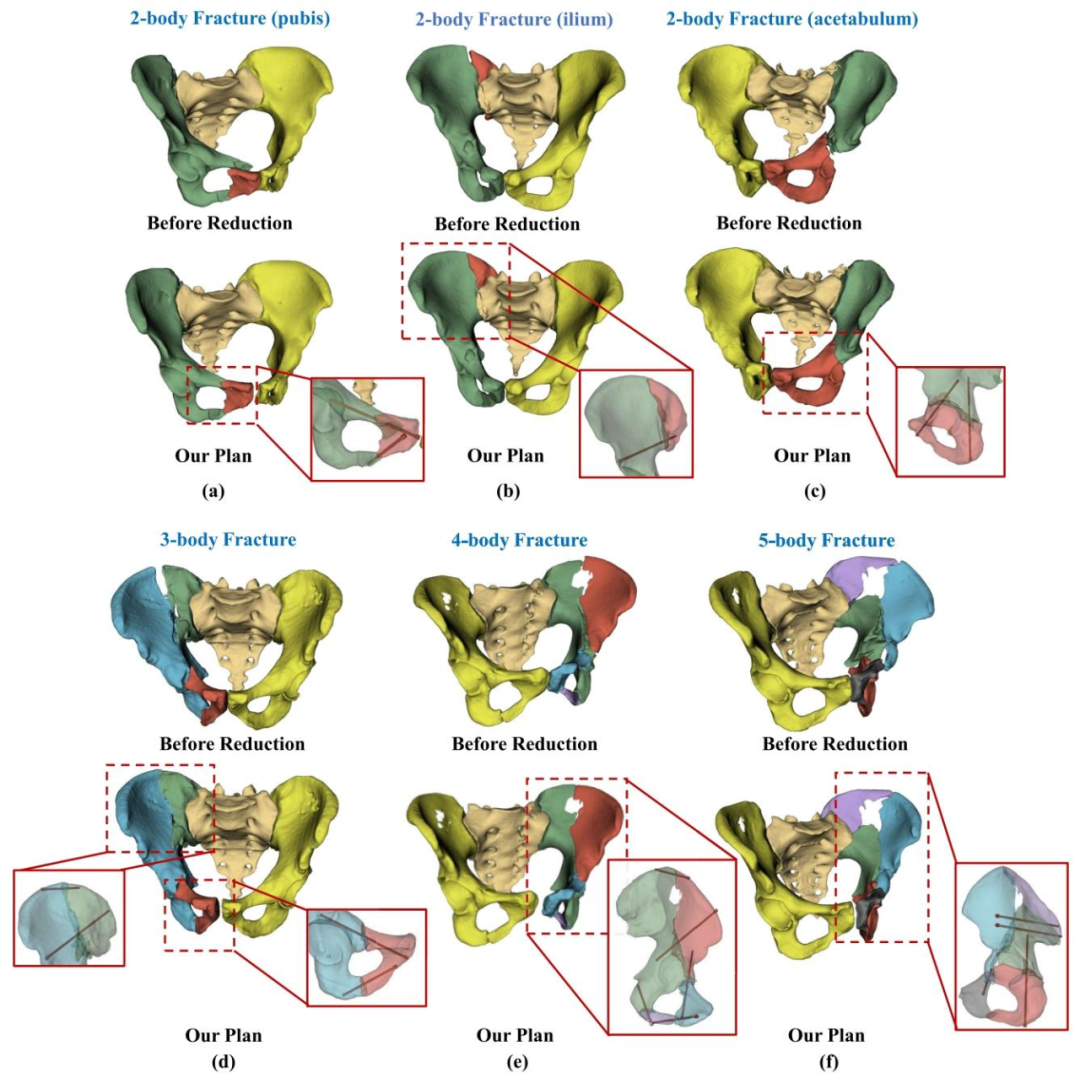
Fig. 11. Examples of various types of pelvic fractures and our preoperative planning results. (a)2-body fracture of the pubis; (b)2-body fracture ofthe ilium; (c)2-body fracture of the acetabulum; (d)3-body fracture of multiple structures; (e)4-body fracture of multiple structures; (f) 5-body fractureof multiple structures
圖11 不同類型骨盆骨折及術前規劃結果示例 - (a):恥骨二體骨折; - (b):髂骨二體骨折; - (c):髖臼二體骨折; - (d):多結構三體骨折; - (e):多結構四體骨折; - (f):多結構五體骨折。
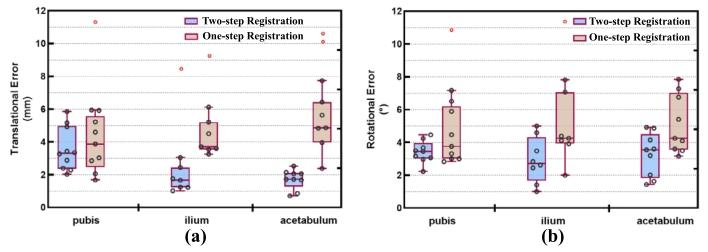
Fig. 12. The reduction error of one-step registration as compared toour two-step registration method for the pubis, ilium, and acetabulum:(a) translational error; (b) rotational error.
圖12 恥骨、髂骨及髖臼部位一步配準與本文兩步配準方法的復位誤差對比 - (a):平移誤差(展示在恥骨、髂骨、髖臼三個解剖部位,一步配準與兩步配準分別產生的平移方向誤差數值對比,直觀呈現兩步配準在降低平移偏差上的優勢); - (b):旋轉誤差(呈現上述三個部位中,兩種配準方法對應的旋轉方向誤差差異,體現兩步配準在提升旋轉復位精度方面的效果)。
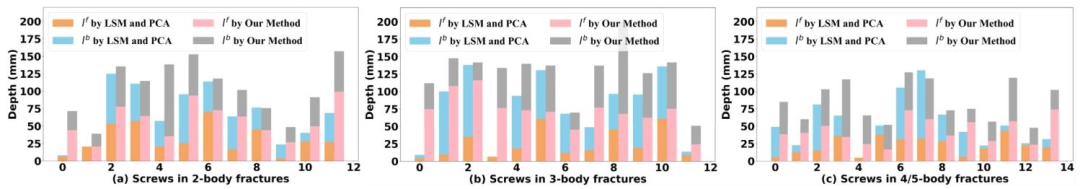
Fig. 13. l f , lb from vr and our method in Section III-D.3: (a) 2-body, (b) 3-body,and (c) 4/5-body fractures.
圖13 基于初始方向(v_r)與本文第III-D.3節方法的(l_f)、(l_b)對比:(a)二體骨折,(b)三體骨折,(c)四體/五體骨折
Table
表
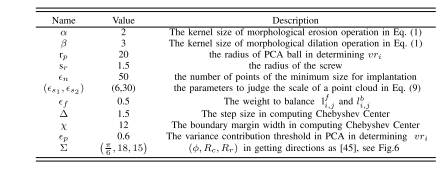
table i parameter setting in the experiment of screw implantation planning
表 1 螺釘植入規劃實驗中的參數設置
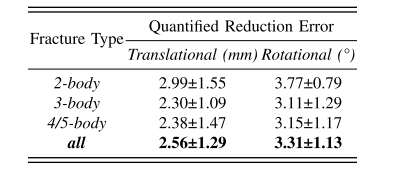
table ii reduction error of clinical cases
表2 臨床病例的復位誤差
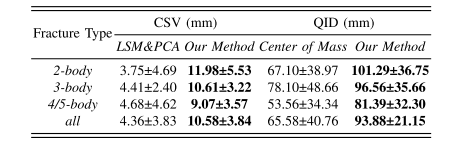
table iii the contrast experiment on qid and csv
表3 QID與CSV的對比實驗
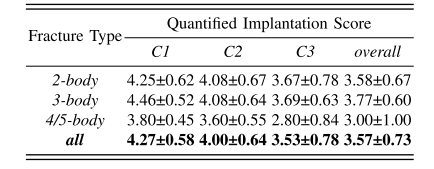
table iv results of the likert rating scale survey
表 4 李克特量表調查結果
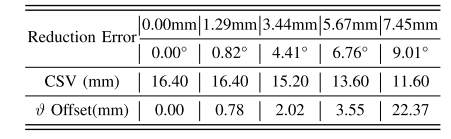
table v the quantified outcomes of implantation planning in a case with different reduction errors. csv was measured with a resolution of 0.40mm
表5 不同復位誤差病例中植入規劃的量化結果 臨床安全價值評分(CSV)的測量分辨率為0.40毫米。
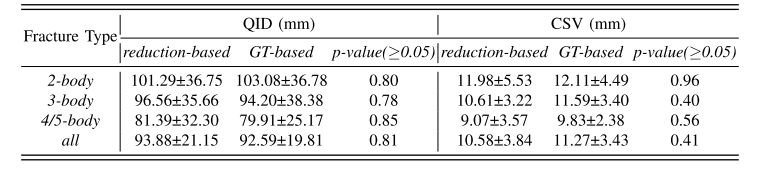
table vi the quantified effects of the reduction planning on implantation
表6 復位規劃對植入規劃的量化影響






。)







)
)



